Leaders in older people’s homelessness
Since our beginning more than 90 years ago, we’ve been at the forefront of innovative approaches for providing homes and support to those who need them most.
Leaders in older people’s homelessness
Since our beginning more than 90 years ago, we’ve been at the forefront of innovative approaches for providing homes and support to those who need them most.
Research and experience support what residents tell us
From homes for destitute families in the Great Depression and cottages for aged ‘battlers’ in the 1950s, our Darlinghurst care home for older people experiencing or at risk of homelessness is now at the forefront of our homelessness services.
Darlinghurst residents self-report a significant improvement in their health, and this is backed by research¹ showing reduced hospital admissions and clinically significant improvements in health-related quality of life and post-traumatic stress syndrome (PTSD).
¹ O’Connor et al., 'An Australian aged care home for people subject to homelessness: health, wellbeing and cost–benefit', BMC Geriatrics (2023) 23:253
Relationship-based, trauma-informed
Our relationship-based philosophy of care includes tailoring care to the unique story of each person, getting to know them and what living their best day looks like. As trauma is common among those who have experienced homelessness, this also informs our evidenced-based approach to care.
What makes our homelessness services different?
When other services end, we begin
Most aged care is not equipped to support people experiencing homelessness, and homelessness services often lack expertise for older people. Our homelessness services bridge these gaps with expertise in both aged care and homelessness, allowing us to welcome the people no one else can, preventing ‘sleeping rough’ or long stays in hospital.
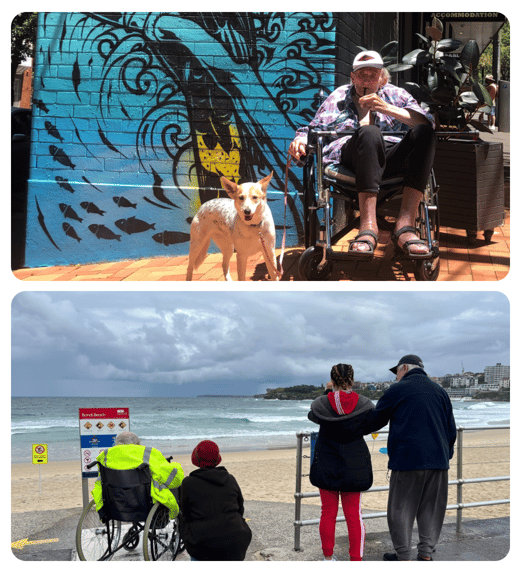
Choice, care and a stable home forever
For many older people who experience homelessness, mistrust of health institutions is a barrier to much needed support. The dignity of choice, meaningful relationships and freedom of movement help new residents embrace a home that is safe and caring, for as long as it's needed.
Loving arms and services 'wrap-around'
Relationship-based care means small, empowered care teams growing to know the same residents over time. It’s not uncommon to hear both residents and the team describe this as ‘family’. Trauma-informed includes recognising the value of wrap-around services such as pastoral care, palliative care, legal, mental health services and alcohol and drug support.
Design that enables independence
Our building design is not only based on research, but more than 30 years’ experience providing small, domestic, familiar and non-institutional care homes, with kitchens and outdoor access, that help maximise resident independence and quality of life. This small-household design was recommended by the Aged Care Royal Commission and is now the preferred aged care approach.
Research and care go hand in hand
Across HammondCare, research closely aligns with the services we provide, as part of our commitment to continual improvement. This is the case for our homelessness services where research projects both inform and learn from the care we provide.
High level care for complex needs
Our focus is to care for those that others can’t or won’t. In homelessness services, this includes filling a significant gap by providing high-level clinical care – including 24/7 nursing support – for complex needs in the context of homelessness, mental health and trauma. Other homelessness services often refer people to us.
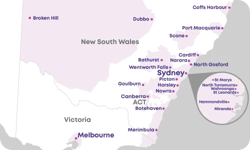
Located where the need is greatest
HammondCare Darlinghurst
Since opening in 2020, the 42-place HammondCare Darlinghurst has supported nearly 130 older people with complex needs, experiencing or at risk of homelessness. Adapting our sector-leading small household design to an inner-city location, we’ve researched each step of our trauma-informed care as we develop further residential services.
As well as offering a safe and stable home, the location near one of Australia’s highest concentrations of older people experiencing homelessness, ensures residents remain connected to the community they are familiar with, so that it’s easier to make a new home and receive care that is much needed.
Alongside a trained, dedicated and empowered care team, the Darlinghurst home maintains strong partnerships with local homelessness, mental health, drug and alcohol and Indigenous support services, the team at St Vincent’s Hospital as well as our own clinical, health and aged care experts. Another key partnership is with St John’s Anglican Church (next door) including Rough Edges.

Future homelessness services
Building on the success of our Darlinghurst care home, we are actively exploring new opportunities for our next specialist care home for older people who are experiencing or at risk of homelessness with complex care needs.
The 2021 Census shows again that older people’s homelessness continues to grow - every night more than 19,378 Australians aged 55 or above are experiencing homelessness, representing one in seven (15.8%) of the overall homelessness population. And this is especially true for the City of Sydney with one of the highest concentrations of older people facing homelessness.
That’s why we remain dedicated to serving this vulnerable community.


"Their only reward is the happiness of people living with the black fear of homelessness hanging over their heads."
Rev Bob Hammond
1933, speaking of why we help people experiencing homelessness.
Finding comfort after lifelong heartache
A proud First Nations woman, Mona is part of the Stolen Generation. Her childhood memories reveal pain, suffering and lifelong heartache. Mona was one of up to 800 older people experiencing homelessness in inner Sydney. At her last hospital admittance, a social worker advocated for Mona to move into HammondCare Darlinghurst.
She says she’s now being looked after and gets the greatest care. When Mona joined us, she had experienced behaviours that impacted her care and had been prescribed antipsychotic medications. Today, living in a safe, comfortable, and loving environment, Mona has developed trusting relationships and knows we have her best interests at heart.
Our team consider it a privilege to get to know Mona, to understand what is important to her and to help her achieve her goals – most notably her successful withdrawal from antipsychotic medications.
Name and photo changed to protect privacy.
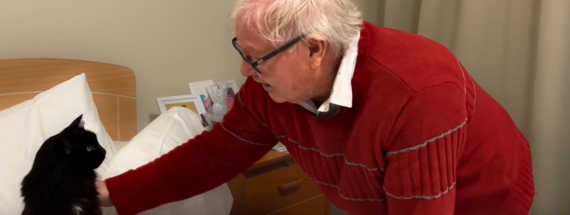
Safe now after being petrified every night
Kenny, aged 82, was reasonably independent and living in a Sydney boarding house. But as this environment deteriorated, he spent a hellish 12 months feeling afraid every night, not being able to sleep until he was no longer able to support himself.
Kenny says he saw the worst you could ever see and so when he was able to move into HammondCare Darlinghurst, he says in his first month ‘I slept practically the whole time’.
As safe as he now felt, he was upset that his much-loved cat Willow, who he’d had for 12 years, was not with him. But once he settled in, Willow came to join him and he (and Willow) feel completely at home. Kenny says, ‘I don’t have one complaint, not one. They have been so nice to me.’
Caring for those in need, regardless of circumstances
Alongside our dedicated older people’s homelessness services, we are committed to improving quality of life for people in need, regardless of their circumstances. Across residential care, home care and health services, we have a long record of supporting the most vulnerable, including those experiencing or at risk of homelessness.
Online support
Our palliative staff specialists
HammondCare’s palliative care services are led by an experienced and respected team of leaders in the field of palliative and supportive care. This includes leading palliative care medical specialists and researchers striving for excellence in clinical care and better outcomes for patients.

Josephine Clayton
Director of Palliative Care Research & Learning, The Palliative Centre

.jpg?width=270&height=249&name=Rectangle%2022%20(1).jpg)
Melanie Lovell
Senior Academic, Palliative Care Research & Learning, The Palliative Centre

.jpg?width=270&height=249&name=Rectangle%2022%20(2).jpg)
Sarah Thompson
Medical Director and Staff Specialist, Neringah Hospital

.jpg?width=270&height=249&name=Rectangle%2022%20(3).jpg)
Amy Chow
Director of Palliative Care, Braeside Hospital and Palliative Care Research Lead at Braeside Hospital, Palliative Care Research & Learning, The Palliative Centre

.jpg?width=270&height=249&name=Rectangle%2022%20(4).jpg)
Abigail Franklin
Staff Specialist, Northern Beaches Hospital

.jpg?width=270&height=249&name=Rectangle%2022%20(5).jpg)
Peter Roach
Staff Specialist, Northern Beaches Community Palliative Care Service

.jpg?width=270&height=249&name=Rectangle%2022%20(6).jpg)
Mariclaire Francisco
Staff Specialist, Braeside Hospital

.jpg?width=270&height=249&name=Rectangle%2022%20(7).jpg)
Victor Sze
Staff Specialist, Greenwich Hospital

.jpg?width=270&height=249&name=Rectangle%2022%20(8).jpg)
Martin Kennedy
Senior Staff Specialist, Community

.jpg?width=270&height=249&name=Rectangle%2022%20(9).jpg)
Dr Shawna Koh
Staff Specialist, Greenwich Community Palliative Care Service

.jpg?width=270&height=249&name=Mask%20Group%20(1).jpg)
Dr Eddy Thientosapol
Staff Specialist, Northern Beaches Hospital

.jpg?width=270&height=249&name=Mask%20Group%20(2).jpg)
Philip Macaulay
Staff Specialist


Dr Wei Lee
Senior lecturer in the USYD Northern Clinical School



Josephine Clayton
Director of Palliative Care Research & Learning, The Palliative Centre
Josephine leads a research program that aims to improve communication between patients, families and clinicians in order to enhance palliative and end-of-life care.
Her research has been published extensively in leading international journals in palliative care and oncology and is widely translated into clinical practice. She also has a strong interest in teaching communication skills relevant to the care of patients with life-limiting illnesses.

.jpg?width=270&height=249&name=Rectangle%2022%20(1).jpg)
Melanie Lovell
Senior Academic, Palliative Care Research & Learning, The Palliative Centre
Professor Melanie Lovell is a Clinical Associate Professor in Palliative Care at the University of Sydney’s Northern Clinical School and Adjunct Professor at the University of Technology Sydney.
Melanie’s research interests include cancer pain, spirituality and translational research. She is widely published and contributes professionally to the executive of the Sydney Institute of Palliative Medicine and the Royal College of Physicians Spirituality Training Curriculum Working Group.

.jpg?width=270&height=249&name=Rectangle%2022%20(2).jpg)
Sarah Thompson
Medical Director and Staff Specialist, Neringah Hospital
With an extensive clinical background, Dr Sarah Thompson has a strong commitment to delivering excellent specialist palliative medicine. Sarah's care is tailored to the individualised needs of each patient and she understands the importance of “living most fully until your last breath.”
Sarah is particularly interested in the importance of hope, meaning and dignity in the palliative care setting, and is involved in undergraduate and postgraduate teaching and mentoring.

.jpg?width=270&height=249&name=Rectangle%2022%20(3).jpg)
Amy Chow
Director of Palliative Care, Braeside Hospital and Palliative Care Research Lead at Braeside Hospital, Palliative Care Research & Learning, The Palliative Centre
Dr Amy Chow graduated from the University of Auckland in 2005 and has worked in various hospitals in New Zealand and Australia ever since. She obtained her Fellowship in Palliative Medicine in 2017 and was appointed to the role of Director of Palliative Care at Braeside Hospital in 2020.
Amy is also the lead in palliative care research at Braeside Hospital. She believes that best practice palliative care should be available widely and would like to ensure patients with palliative needs have dignity and quality of life at the end of life.

.jpg?width=270&height=249&name=Rectangle%2022%20(4).jpg)
Abigail Franklin
Staff Specialist, Northern Beaches Hospital
Dr Abbie Franklin graduated from Edinburgh University with Honours in 2000 and was awarded the Dorothy Gilfillan Prize for the highest-ranked female graduate. After initial training in surgery in Scotland, Abbie moved to Australia and gained further experience in critical care, general medicine, emergency medicine and psychiatry.
Abbie went on to complete training in general practice in Sydney and Bathurst and was awarded the Iris and Edward Gawthorn Award from the Royal Australian College of General Practitioners. Abbie then completed training in palliative medicine, including undertaking a pain fellowship at the Royal Prince Alfred Hospital, and a research project looking into advance care planning in primary care.

.jpg?width=270&height=249&name=Rectangle%2022%20(5).jpg)
Peter Roach
Staff Specialist, Northern Beaches Community Palliative Care Service
Dr Peter Roach graduated from medicine at UNSW in 2004. After working in hospitals, Peter obtained diplomas in Children's Health and Palliative Medicine. He then trained as a GP in Western Sydney and Tamworth. After working as a GP in Northern Sydney, Peter then commenced specialist palliative care training in 2016.
Peter now works as a Palliative Care Specialist in the community on the Northern Beaches. His research project while training in palliative care focused on the palliative care needs of those with dementia.

.jpg?width=270&height=249&name=Rectangle%2022%20(6).jpg)
Mariclaire Francisco
Staff Specialist, Braeside Hospital
Dr Mariclaire Francisco earned her MD and completed a three-year residency in internal medicine at the University of the Philippines Manila, before arriving in Perth in 2008, where she began physician training with the RACP.
Mariclaire completed her training in geriatric medicine and earned her FRACP in WA in 2016. She then moved to Adelaide for post-fellowship training in palliative medicine, where she was awarded her FAChPM. In 2019, she joined the Braeside palliative care team as a Staff Specialist in Palliative Medicine.

.jpg?width=270&height=249&name=Rectangle%2022%20(7).jpg)
Victor Sze
Staff Specialist, Greenwich Hospital
Dr Victor Sze graduated with an MBBS from the University of NSWs in 2004. He has since worked as a palliative care staff specialist in acute care hospitals, inpatient palliative care units and the community across the South Eastern Sydney, South Western Sydney and Northern Sydney Local Health Districts since 2016.
Victor joined HammondCare in 2019. His work in the palliative care unit encompasses providing best practice symptom management to improve quality of life and support for patients and their families.

.jpg?width=270&height=249&name=Rectangle%2022%20(8).jpg)
Martin Kennedy
Senior Staff Specialist, Community
Dr Martin Kennedy is a Palliative, Pain and Rehabilitation Medicine Physician and a Staff Specialist in palliative medicine for HammondCare, with conjoint appointments at Sydney, NSW and Macquarie Universities.
Martin has more than 25 years of experience in specialist sub-acute medical care, and for over 15 years has worked right across Northern Sydney in public and private acute care hospitals, inpatient and outpatient palliative care, rehabilitation units and the community.

.jpg?width=270&height=249&name=Rectangle%2022%20(9).jpg)
Dr Shawna Koh
Staff Specialist, Greenwich Community Palliative Care Service
Dr Shawna Koh graduated from the University of Auckland in 2007 with MBChB and Honours. She completed palliative care specialist training with the Royal Australasian College of Physicians in 2016 and joined HammondCare as a Palliative Care Staff Specialist.
Shawna completed a research project, which was part of a Research Masters with the University of Notre Dame Sydney, examining the use of end-of-life care pathways in tertiary hospitals.
She is passionate about providing evidence-based holistic care in the community to improve symptom management and quality of life in patients with life-limiting illnesses.

.jpg?width=270&height=249&name=Mask%20Group%20(1).jpg)
Dr Eddy Thientosapol
Staff Specialist, Northern Beaches Hospital
Dr Eddy Thientosapol graduated from UNSW Medicine in 2005 and completed physician training in medical oncology at Royal Prince Alfred Hospital in 2013. He also completed a Master of Clinical Epidemiology from the University of Sydney in 2016.
In 2017, Eddy was awarded a Fulbright Scholarship and spent one year at the Molecular Immunology Laboratory at Rockefeller University, New York. He was awarded a PhD by the University of Sydney in 2019.
Eddy completed post-fellowship palliative care training in 2020. He then joined HammondCare providing consultation services at Northern Beaches Hospital and the Southern NSW Local Health District.

.jpg?width=270&height=249&name=Mask%20Group%20(2).jpg)
Philip Macaulay
Staff Specialist
Philip has enjoyed over 30 years working in palliative care, managing both community and inpatients as a staff specialist.
He has worked in many areas of Sydney, enjoying the diversity that both his patients and colleagues have brought. He believes in collaborating to achieve the best outcome for patients’ holistic care.
Throughout his career, Philip has participated in research, conferences and education, taking an active role in facilitating the next generation in this field.
Philip has completed a Graduate Diploma of Divinity and sees education as a life-long learning experience.


Dr Wei Lee
Senior lecturer in the USYD Northern Clinical School
Dr Wei Lee is a Staff Specialist Physician in palliative medicine in Northern Sydney and a Senior Lecturer in the University of Sydney Northern Clinical School. He is the coordinating principal investigator for SKIPMDD – a phase II pilot feasibility study exploring the use of subcutaneous ketamine infusion in palliative care patients for major depressive disorder.Wei is on the Palliative Care Clinical Studies Collaborative Trials Management Committee and Cancer Symptom Trial Scientific Committee. He is also the early career researcher representative on the Palliative Care Clinical Academic Group of Sydney Partnership for Health, Education, Research and Enterprise (SPHERE).